An advance directive instructs medical staff on how you do (and don’t) want to be treated if you become incapacitated and are no longer able to speak for yourself. One of the primary aspects of your advance directive will normally include resuscitation orders and whether you’re a “full code” patient open to different forms of resuscitation.
Read on to find out what a full code status is, how to outline your wishes in an advance directive, and why it’s essential to share that full code directive.
Key Takeaways
A full code advance directive is a legal document giving doctors permission to use all forms of resuscitation if you stop breathing or your heart stops beating.
Medical patients in the U.S. are normally treated as full code patients unless their advance directives state otherwise.
Patients can generally pass on a full code directive verbally, by creating a living will, or through a healthcare power of attorney.
What Is a Full Code Advance Directive?

A full code advance directive is a document to ensure your medical care providers know what sort of treatment you’d like to receive in the event you cannot communicate your own wishes.
When a patient goes “full code,” it means their heart has stopped beating or they’ve stopped breathing. In these instances, a medical team might pursue several different measures to resuscitate a coding patient.
For example, they might use defibrillation, perform chest compressions, or deploy intubation. These methods all fall under the umbrella of cardiopulmonary resuscitation (“CPR”).
It’s worth pointing out that full code is generally the default code status for patients. Unless you’ve created an advance directive stating otherwise, your medical team will normally perform all available actions to resuscitate you.
That being said, some patients choose to spell out their wishes to receive all forms of resuscitation by completing a full code advance directive.
Related: Common Types of Advance Directives
How Does an Advance Directive Work?

An advance directive is a legal document, and doctors are required to honor the wishes of your advance directive in most instances.
For medical teams, they provide crucial instructions outlining the treatments you do and do not want to receive. For patients, advance directives provide a way to communicate with care providers in the event you can’t speak for yourself or are too ill to make an informed decision.
Although rules on advance directives vary by state, you’re generally given the choice to create one of two types of advance directives: a living will or a healthcare power of attorney.
David Brillant, founder of Brilliant Law Firm explains:
“Each serves different purposes. A living will dictates your wishes regarding medical treatment if you become incapacitated, while a durable power of attorney for health care appoints someone to make medical decisions on your behalf.
The choice between these can often depend on individual circumstances and preferences, highlighting the importance of personalized legal guidance.”
It’s not required to have an attorney’s help to draft your advance directive.
However, some states have laws around who can witness an advance directive and whether it needs to be notarized to become valid. It’s worth chatting with a lawyer or estate planner to ensure your advance directive meets the requirements in your state of residence.
An advance directive is legally recognized, but it’s not legally binding.
When a valid advance directive is communicated to your medical team, doctors are required to do their best to honor your directive. However, there may be some instances in which they can’t follow your wishes precisely.
What’s the Difference Between a Full Code Directive and a DNR Directive?
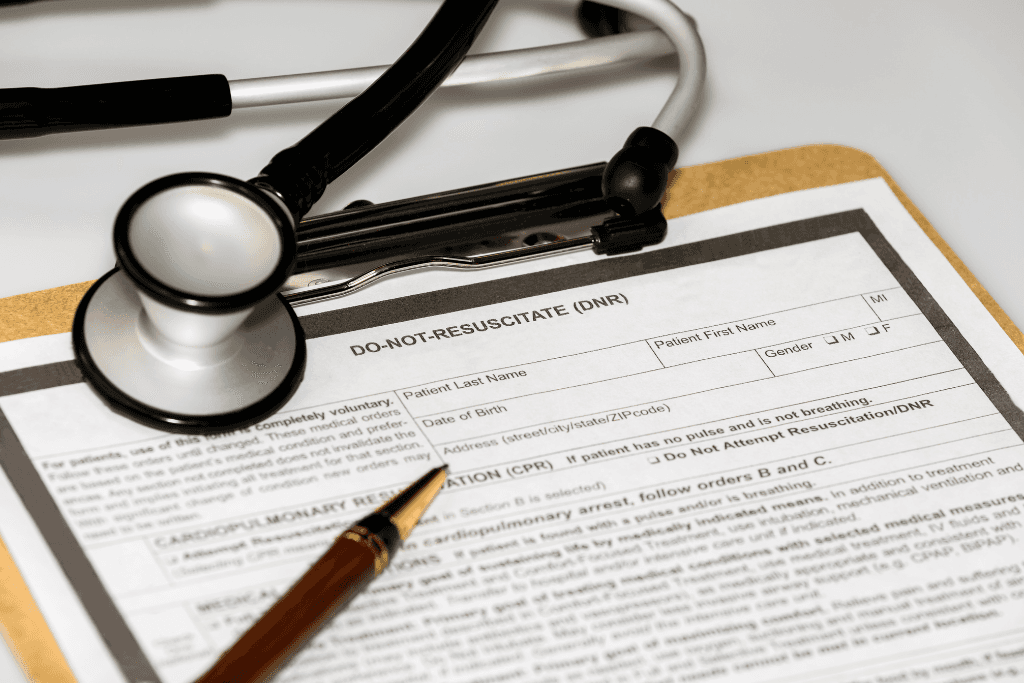
Advance directives can be as specific as you’d like them to be. But generally speaking, patients will normally use a directive to opt for or against three different treatment scenarios:
As we’ve already mentioned, a full code is when a patient stops breathing, their heart stops beating, or both occur simultaneously. With a full code directive, your care providers can use any means of resuscitation available to them.
The default status for most patients in the U.S. is full code. As a result, you can expect healthcare providers to take every possible action to resuscitate you in the event that your great stops or you’re unable to breathe.
A DNI directive instructs medical staff that it’s ok to perform CPR if your heart or breathing stop, but you do not want a breathing tube to be involved in your resuscitation.
If you create a DNR advance directive, you’re telling doctors that you don’t want CPR attempted in the event that your heart stops or you stop breathing, even if resuscitation is an option that’s available to the doctors who are treating you.
Each advance directive is unique and designed to express the wishes of individual patients.
This choice could stem from personal wishes, relationship situations, or religious beliefs. Either way, spelling out your wishes within a legal document ensures they’re communicated to doctors and honored wherever possible.
How Do You Create a Full Code Advance Directive?

The process for creating a full code advance directive depends on the type of directive you choose to pursue.
Because patients are normally treated as full code unless they communicate otherwise, a full code directive doesn’t normally have to be written or notarized. All you’ve got to do is tell your doctor you’re open to all forms of resuscitation, and they should update your medical records accordingly.
That being said, it’s possible to include a full code directive in your living will or healthcare power of attorney.
In most states, a living will does not need to be notarized but witnesses may be required. By contrast, a healthcare power of attorney will typically need to be both notarized and witnessed. As a result, it’s worth speaking with your lawyer or estate planner to chat about the process, requirements, and what might be the best option for you.
Regardless of the directive you end up going for, your final step must be to communicate the wishes of that directive to loved ones.
Alana Gibson, Chief Operating Officer of DGR Legal advises:
“It's essential to share your advance directive with your family, health care proxy, attorney, and healthcare providers to ensure your wishes are respected and accessible when needed.”
That’s where platforms like Trustworthy can go a long way towards supporting patients and their families.
Trustworthy is a Family Operating System® that allows you to create, store, and manage all the important documents in your life. Using our intelligent digital vault, you’re able to upload documentation like a full code directive and create an encrypted digital copy.
From there, you can securely store your directive and grant viewing access to people like your spouse, children, doctor, or estate planner to ensure everyone in your life has the ability to see and understand your medical wishes.
This prevents family disagreements and uncertainty in the future and guarantees everyone is on the same page moving forward.
Ready to learn more? Check out Trustworthy’s range of security features to discover how it can support your family.
Frequently Asked Questions
What does it mean when a patient is full code?
A medical patient is considered “full code” if their heart stops beating, they stop breathing, or both issues occur simultaneously.
Can I change my mind about my full code status in my advance directive?
Yes, you can modify your advance directive at any time as long as you have decision-making capacity. If your wishes change, complete a new advance directive form and provide updated copies to your health care agent, loved ones, and medical providers. Be sure to destroy any old versions.
Will emergency responders honor my full code advance directive?
In an emergency situation, first responders like paramedics will attempt full resuscitation efforts unless they are aware of a valid physician-signed DNR order. Your advance directive may not be immediately available to emergency personnel. Consider discussing your full code status with your doctor.
We’d love to hear from you! Feel free to email us with any questions, comments, or suggestions for future article topics.
Trustworthy is an online service providing legal forms and information. We are not a law firm and do not provide legal advice.